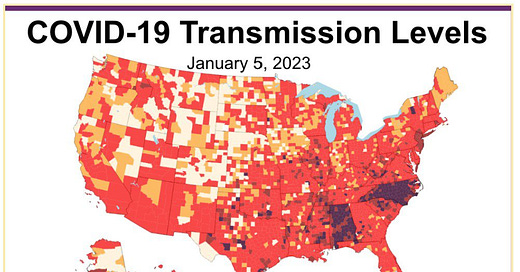
The Weather: Transmission levels remain high, with 98.3 percent of the population living in areas with substantial or higher transmission. Rates are particularly high along the East Coast & Southeast, with lower levels in the West.
On Variants: The most common variants (55%) remain BQ1/1.1. Last week, a new variant, XBB1.5 (Kraken) was first reported. These variant reports use models to estimate each variant – this week’s model suggests 28% of cases are due to XBB1.5. It is dominant in the Northeast.

What we know:
– XBB1.5 was first detected in New York state
– It spreads faster than other variants & will likely reach the entire US shortly
– It evades prior immunity – but there is likely still benefit from the bivalent booster
What we know:
– While monoclonal treatment/prevention no longer works against newer variants, Paxlovid still should work.
– High quality masks, ventilation, & testing all still reduce risk of infection.
What we don’t know:
– Whether XBB1.5 causes more severe disease. It’s worth remembering that variants with high transmission can put more people in the hospital even if they are not more severe.
There are large differences regionally – which may explain differences in hospitalizations – with XBB1.5 (dark purple) the most common variant in the Northeast and growing in the South. Most other regions have BQ1/1.1 (teal greens) as the most common.

Wastewater Monitoring: National wastewater levels remain high – again, higher than any winter peak before Omicron.

Regionally, wastewater levels are highest in the Northeast, with increasing levels in the South. Levels are the lowest in the West – though data appears to be missing for this week.

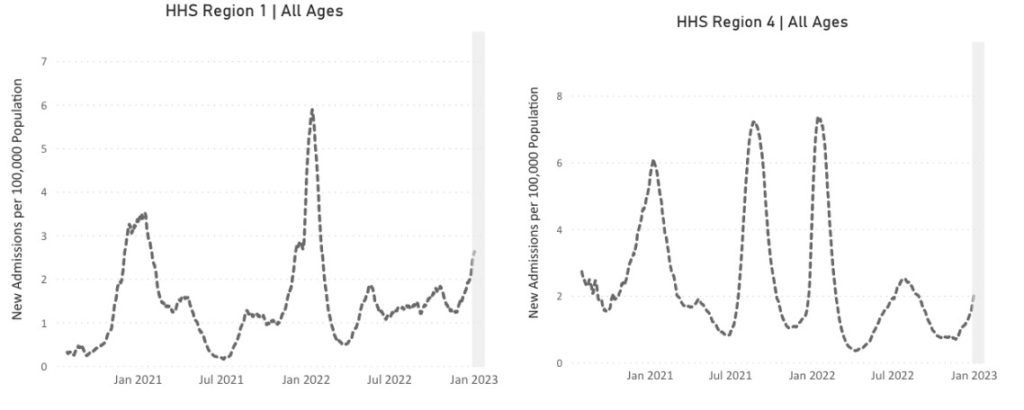
Hospitalizations: Hospitalizations are increasing, with particularly high rates among those over 70, rivaling the peak of the Delta wave.

Hospitalizations are also increasing in the Northeast (for example Region 1) and the South (Region 4).
Deaths: The week of January 4, at least 2,731 people died of COVID nationally. At least 254,124 people died of COVID in 2022. This was the third year of the pandemic – a year when we supposedly had “the tools necessary” to control COVID.
COVID is clearly NOT the flu – 254,124 deaths is 5 times more than the worst year of flu deaths in the last decade. Over the course of the entire pandemic, 1,600 children have died of COVID.
Globally, the U.S. has a higher rate of COVID-19 deaths than many of our peer nations, yet there is no sense of urgency from the federal government to do much other than rely exclusively on vaccines. Universal booster shots, masking, and clean air are critical.

Long COVID: A comprehensive meta-analysis of Long COVID was published & shows 45% of COVID survivors, regardless of hospitalization, were experiencing unresolved Long COVID symptoms after 4 months. Similar symptoms are being reported whether from Omicron or Delta variant.
Our kids are not okay. The findings in the aforementioned meta-analysis show a “significant proportion of seropositive children, particularly adolescents, experiencing persistent COVID symptoms.”
Another study states “The majority of children who develop persistent dyspnea after COVID infection exhibit reversible peripheral airway obstruction and lung hyperinflation despite normal spirometry.”
As peripheral airways cannot always be seen with standard pulmonary tests, there is an extra need to watch out for this to make sure our kids are diagnosed and treated correctly.
Speaking of treatments, a new study offers some insight into Long COVID, finding that there are four major subtypes of Long COVID, a critical piece of information as clinicians try to prescribe relevant treatments. They are as follows:
34% have heart, kidney, & circulation-based symptoms; risk of heart failure post-COVID is almost doubled
33% have respiratory & sleep problems, anxiety, headache & chest pains
23% have musculoskeletal & nervous system symptoms
10% have combined digestive & respiratory symptoms
Forecast: There is no room for complacency on COVID in 2023. The global community must invest in and strengthen our public health systems to handle the dramatic increases in hospitalizations, reduce COVID transmission, and protect people from Long COVID.
A recent study post-Omicron has demonstrated that vaccines have a small effect on reducing transmission. While the study was done in a prison setting, it is noteworthy because there have been few studies on transmission in the era of Omicron.
Paxlovid is a critical treatment yet its distribution and usage remain structurally limited: Black and Hispanic populations are 30-36% less likely to be prescribed Paxlovid than white populations. Health officials must do better.

For example, now is not the time to remove Paxlovid subsidies, yet by mid-2023, Paxlovid will hit the private market and cost hundreds of dollars, making it significantly less accessible to those who need it most.
Take Action: The updated booster is still an important layer – yet, nationally, only 15% of the public and 38% of seniors have gotten the bivalent vaccine – with particularly low rates in the South. Please get your bivalent vaccine booster now to protect you and your loved ones.

Caring for each other in our communities is essential to surviving this pandemic, and yet pandemic scapegoating has increased hate against Asian Americans and Native Hawaiians, with about 28% experiencing or witnessing a hate incident in 2020-2021.
Report hate crimes and demand that your local representatives uphold resolutions against hate.
Notes: 1) The numbers in this report were current as of 1/6. The CDC updates data frequently as it receives refreshed information. Today’s numbers may be slightly different from the data here. 2) Check out the links throughout & see our website for more! https://peoplescdc.org.